How Weather Affects Joint Pain: Debunking Myths and Finding Relief
Published September 2025
Many people swear their joints can predict the weather. Grandparents often say their knees ache before a storm, and people with arthritis notice flare‑ups when the temperature drops. Yet scientists still debate whether the atmosphere really triggers joint pain. This article explores how barometric pressure, temperature and humidity may influence joint discomfort, reviews the latest research and offers practical tips for coping.
Can the Weather Really Trigger Joint Pain?
Anecdotes about weather‑related joint pain abound, but researchers haven’t established a consistent cause‑and‑effect relationship. Harvard Health explains that while many people insist they can predict the weather based on aches, research has yet to confirm a definitive link. Studies of osteoarthritis show conflicting results: some surveys report more pain when temperature drops and barometric pressure falls, yet large analyses of millions of health‑care visits show no association at all.
A systematic review highlighted that two‑thirds of people with joint pain report weather‑related discomfort, but it also found no “perfect” climate where everyone feels better. People with osteoarthritis, rheumatoid arthritis, synovitis or past joint injuries appear more sensitive to weather changes than the general population.
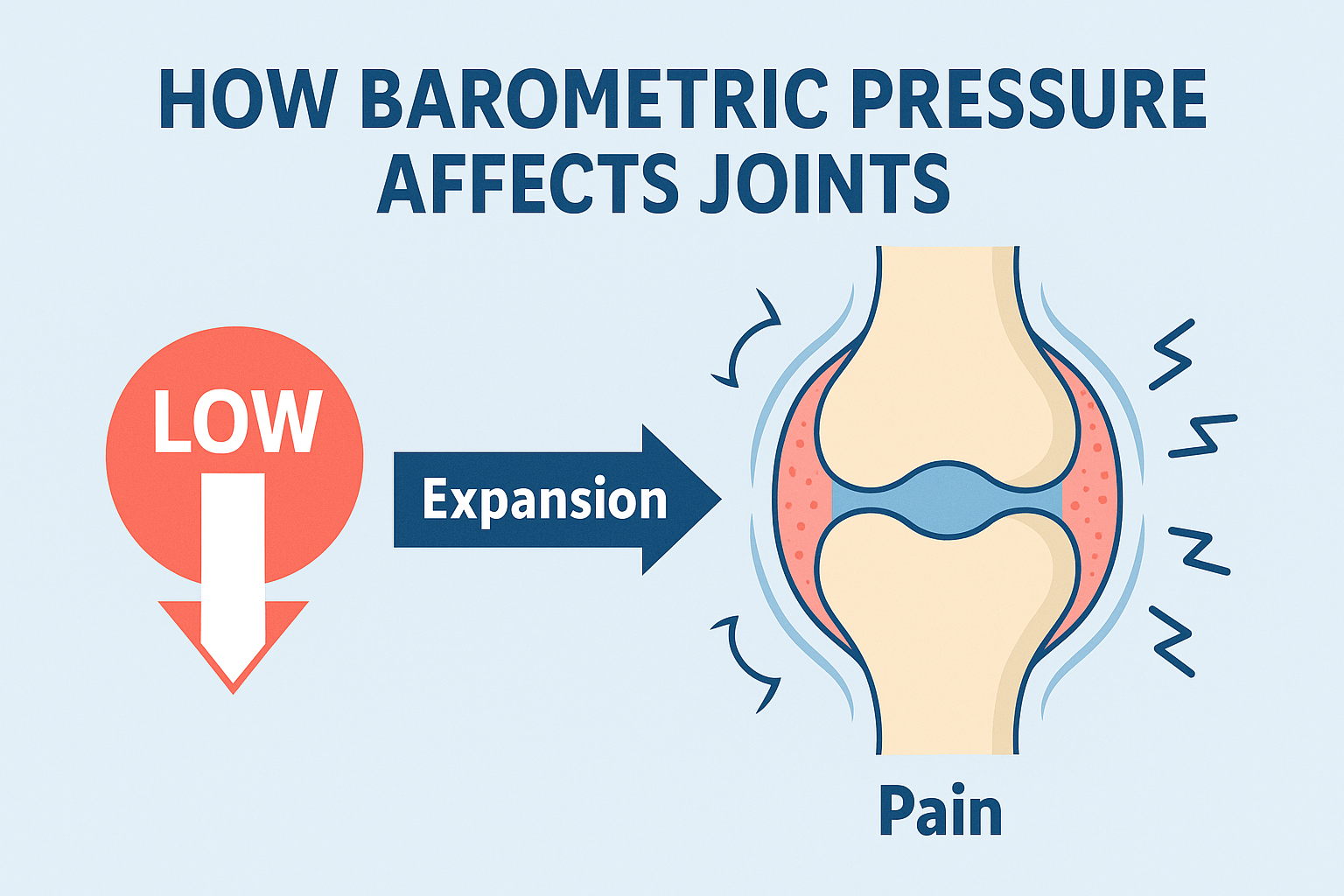
How Barometric Pressure Affects Joints
When a low‑pressure system approaches, the weight of the air pressing against the body decreases. Harvard Health notes that lower barometric pressure allows muscles, tendons and other tissues around joints to expand. That expansion can put pressure on the joint capsule and nearby nerves, potentially leading to pain.
Orthopedic surgeons at RWJBarnabas Health liken joints to barometers: when air pressure drops, bones, muscles and tendons may expand slightly, increasing pressure inside joints. A Tufts University cadaver study found that the ball of a hip joint shifted about one‑third of an inch when barometric pressure decreased. This mechanism could explain why some people feel discomfort before a storm.
Interestingly, not all pressure changes cause pain. A Dutch cohort study of hip osteoarthritis reported increased pain and stiffness when barometric pressure and humidity rose, not when they fell. Researchers therefore think it isn’t the direction of the change that matters so much as how quickly pressure fluctuates.
Temperature: Cold Weather and Joint Stiffness
Cold temperatures often make muscles, tendons and ligaments stiffer. Nuvance Health notes that cold weather can cause supporting tissues around joints to become less flexible and slow blood circulation, reducing warmth and exacerbating pain. Cedars‑Sinai rheumatologist Mariko Ishimori, MD, compares synovial fluid to motor oil: it thickens like sludge when it’s cold, making joints less nimble.
Some studies suggest that pain worsens with falling temperatures. A survey of knee osteoarthritis patients found that every 10‑degree drop in temperature corresponded to an increase in pain when barometric pressure was low. However, other large studies found no such link.
Humidity and Rain
High humidity and damp conditions may contribute to joint discomfort. Nuvance Health explains that humid weather can make it harder for the body to regulate temperature, leading to stiffness and increased pain. Changes in humidity may also alter how pain signals are perceived. A Dutch study found that pain and stiffness worsened with rising barometric pressure and humidity.
In the United States, many patients report feeling worse on wet or rainy days. The Mount Sinai Health System writes that cold weather tightens muscles and ligaments while humid weather can cause swelling and increased pain. Therefore, it may not be the moisture itself but the way humidity affects body tissues.
Lifestyle and Behavioural Factors
Not all joint pain in winter is due to the weather itself. Inactivity and behaviour patterns play a role. On cold or rainy days, people tend to stay indoors, sit on the couch and move less. Inactivity allows joints to stiffen and muscles to weaken, increasing discomfort. Houston Methodist notes that less activity leads to muscle weakness and inflammation and that pain discourages movement, starting a vicious cycle.
Psychological factors can also amplify pain. Harvard Health notes that expecting discomfort when the weather shifts may make you notice aches more readily. Additionally, bad weather can affect mood, stress levels and sleep patterns, which in turn can make pain feel worse.
Stress, Inflammation and Pain Perception
Cold and damp conditions increase physical stress on the body and heighten inflammation. Nuvance Health explains that such conditions raise inflammation levels, intensifying joint pain. Frigid temperatures can heighten pain sensitivity, slow blood circulation and cause muscle spasms. In arthritic joints, nerves may react more strongly to pressure changes because the protective cartilage is worn away.
Patients should also be aware that prolonged stretches of rainy or cloudy weather can lower mood. According to Mount Sinai, two‑thirds of people with joint pain report weather‑related discomfort, but there is no climate that eliminates pain completely.
Scientific Evidence: A Mixed Picture
The scientific literature offers contradictory evidence about weather’s impact on joint pain. Smaller surveys of osteoarthritis patients often find correlations between lower temperatures or barometric pressure and increased pain. Some research indicates that pain worsens when humidity and pressure rise. Yet large retrospective analyses of millions of patient visits and several Australian studies report no significant association between weather changes and joint pain.
These inconsistencies likely stem from differences in study design and the subjective nature of pain. Many studies rely on self‑reported pain diaries, which can be influenced by expectation and mood. Moreover, weather effects may vary by individual. People with osteoarthritis, rheumatoid arthritis or prior injuries are more likely to be sensitive to changes in weather, while others notice no difference.
Coping Strategies and Practical Tips
Even if researchers haven’t reached a consensus, many people find that managing environmental and lifestyle factors helps reduce weather‑related joint pain. Here are evidence‑backed strategies:
- Keep warm: Dress in layers, use heating pads, electric blankets or warm baths to maintain body warmth. Cedars‑Sinai suggests electric blankets and hot baths to loosen stiff joints.
- Stay active: Low‑impact exercises such as walking, swimming, yoga, Pilates, tai chi or stationary biking keep joints flexible and muscles strong. Warm up with gentle stretches before outdoor exercise.
- Maintain a healthy weight and diet: Being overweight adds stress to joints; losing weight can reduce pain. Eat anti‑inflammatory foods rich in omega‑3 fatty acids (fish, nuts, seeds) and limit sugars and refined carbs.
- Stay hydrated: Drinking plenty of water helps lubricate joints and reduce inflammation.
- Use supportive aids: Compression sleeves provide warmth and stability to sore joints. Paraffin baths or heat/cold therapies can soothe hands and feet. NSAIDs may help reduce inflammation, but consult a doctor before use.
- Consult a healthcare provider: If pain persists, seek medical advice. A physical therapist can design exercises and stretches tailored to you. Doctors may recommend medications, injections or, in severe cases, surgery.
- Check vitamin D levels: Vitamin D deficiency contributes to bone loss and may worsen arthritis pain; ask your doctor to test your levels.
- Watch your footing: Wear appropriate footwear and be cautious on icy or slick surfaces to avoid falls.
Conclusion
While there is still debate about whether weather truly causes joint pain, many people with arthritis and other joint conditions experience flare‑ups when the weather changes. Scientific studies are inconsistent, but theories involving barometric pressure, temperature, humidity and behavioural factors offer clues. What is clear is that staying warm, active and healthy, combined with good self‑care and professional support, can help you ride out the storm and reduce weather‑related joint pain.